13
nmdental.org
the implant without a quality guide. A
quality guide usually cannot be made
with just the information gathered from
a single dental cast. Mounted diagnostic
models, radiographic data and clinical
photos are often necessary to have a
positive, predictable outcome. Modern
technology has taken most of the guess-
work out of implant planning and place-
ment. Most surgical offices now have
3D imaging (Cone Beam CT Scanners)
in their offices that allow very accurate
measurements and planning to be made
before the day of the surgery. There are
various forms of software that can allow
digital data to be converted into a precise
surgical guide (See Figure 4) based on
the prosthetic plan, when indicated,
for a relatively low cost (a few hundred
dollars).
While it is tempting for us as restorative
dentists to blame our surgical counter-
parts when an implant is placed improp-
erly, it is important to remember that we
now live in an era of restoratively-driven
dentistry and that we must take respon-
sibility of the overall restorative plan
for our patients. With modern grafting
techniques, no longer do we have to say
“Well, that was where the bone was, so
that’s where we placed the implant.”
Even when we don’t expect that hard
or soft tissue grafting will be required,
we are wise to spend one or two extra
minutes on the front end explaining to
the patient that possibility so that they
are prepared emotionally and financially
for that journey should it be necessary to
achieve ideal placement. That discussion
is much easier than one regarding implant
removal due to iatrogenic placement.
2
Inadequate restorative
space/improper implant
depth
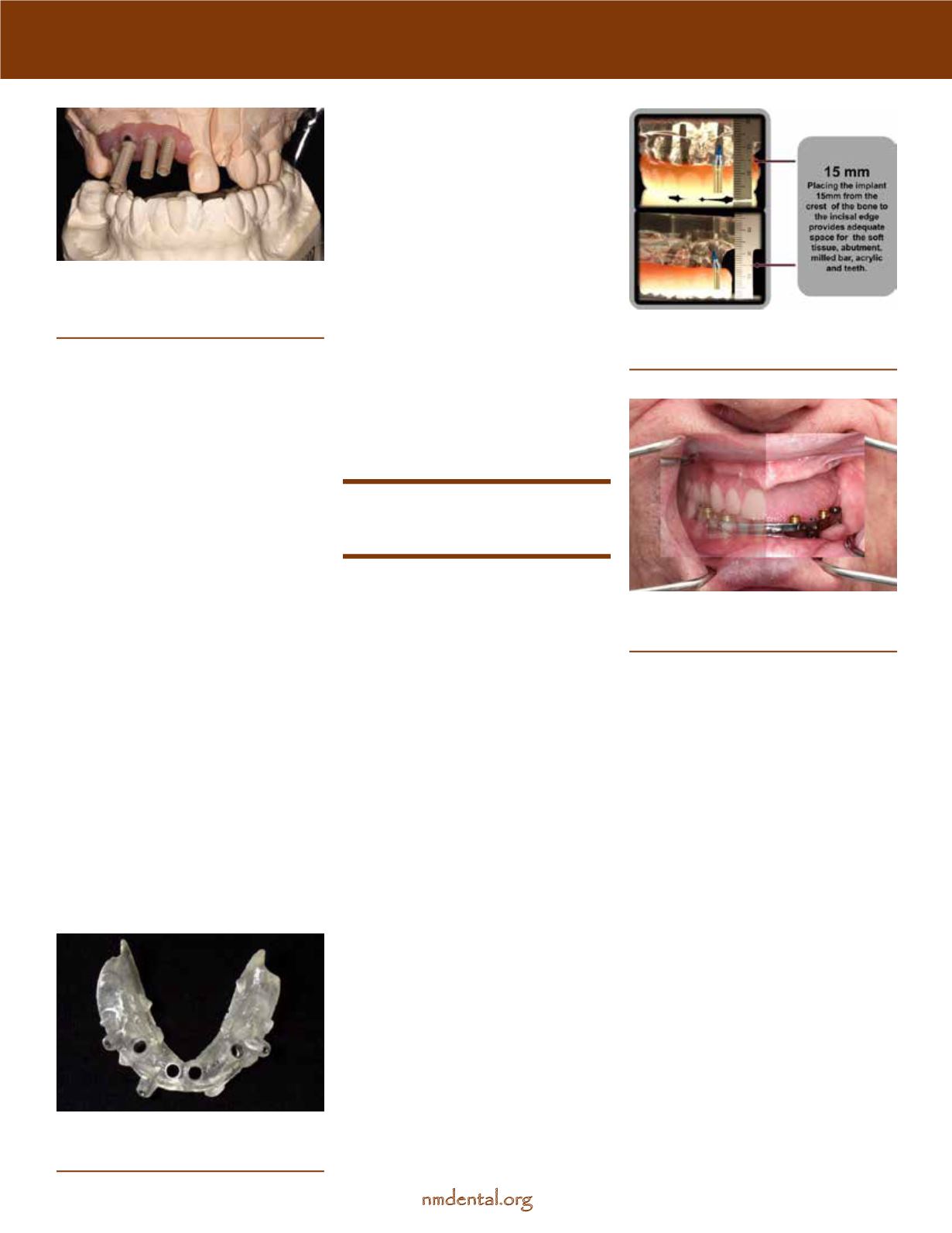
Along with improper implant angle, a
common implant complication is when
the placement is either too superficial
or too deep, with the former being
an immediate problem and the latter
being a potentially significant long-term
problem if the adjacent tooth is lost.
Sufficient restorative space is required for
all successful restorations. The amount
of space needed varies depending on
the restoration. Some overdenture
cases require as much as 15-18 mm (See
Figures 5 and 6) of restorative space
(measured from the implant platform to
the incisal edge) while others may only
require as little as 8-10 mm. It is impor-
tant to communicate to the surgeon
what the prosthetic plan is and how
much space is needed for a successful
restorative outcome.
Additionally, it is of extreme importance
in the esthetic region to make sure that
sufficient space is left to create a proper
emergence profile and avoid exposure
of the implant platform. An implant
placed too superficially will not only be
an esthetic failure, but may also lead to
increased plaque retention next to the
implant or adjacent teeth.
Solution: Plan with the future in mind.
Implant position and placement will
vary according to the final prosthesis.
If necessary, perform wax-ups, virtual
modeling, or even mockups so that both
surgical and restorative teams are on
the same page before the day of surgery.
Always consider contingency plans if
therapy is unsuccessful and anticipate
future treatment the patient may need.
Important note: The level of the bone
of the adjacent teeth will greatly deter-
mine the final level on the implant, but
if the adjacent natural tooth is lost at a
later date, and the implant was placed
deep, the bone will eventually recede to
the level of that implant. This can spell
disaster for a smile if this occurs at a
central-lateral or lateral-canine position.
Figure 3
—Implant model with waxing
sleeves over angled implants. Surgery was
performed without a surgical guide and
without a definitive restorative plan.
Figure 4
—Stereolithographic surgical
guide designed for precisely “guided”
implant placement.
Fig 5
—Diagram illustrating required
restorative for a fixed hybrid bridge
(acrylic and titanium).
Fig 6
—Image showing a patient wearing
an implant bar over denture. Note the
need for inter-arch restorative space.
continues











