New Mexico Dental Journal, Spring 2015
8
It is important to note that not all necrotic, immature teeth are
candidates for this procedure. The AAE has developed some
clinical considerations prior to initiating a pulpal regenerative
procedure. These considerations include:
1) Tooth with a necrotic pulp and immature apex
(apex greater than 2mm in diameter).
2) Pulp space is not needed for post/core or final
restoration.
3) Compliant patient/parent.
4) Patient not allergic to medicaments and antibiotics
necessary to complete treatment.
If these criteria are met, the AAE has developed a treatment
protocol entitled “AAE Clinical Considerations for a Regen-
erative Procedure“. This treatment protocol can be accessed at
the following web address:
www.aae.org/Dental_Professionals/
Considerations_for_Regenerative_Procedures.aspx
.
The following is a brief summary of the treatment protocol
from the AAE website:
A typical regenerative endo procedure is usually two or
more visits, with the first visit focusing on endo access
and disinfection of the pulp space followed by the
placement of an intracanal medicament for 1–4 weeks.
Little to no canal instrumentation is performed.
During the second visit, the practitioner verifies the
absence of clinical signs and symptoms, after which
he or she removes the intracanal medicament. Growth
factors are then released from the dentin walls using
EDTA, delivering cells into the canal space by simu-
lating bleeding into the canal, creating a scaffold
(blood clot etc), and placing a pulp-space barrier such
as MTA or glass ionomer. This is followed by place-
ment of a permanent restoration.
Clinical and Radiographic Follow-up
Perhaps the most rewarding aspect of performing pulpal regen-
erative procedures is monitoring progress at future recall visits.
Typically a practitioner will see:
• Resolution of apical radiolucencies within
6–12 months following treatment.
• Increased width of root walls and increase in
root length 12–24 months following treatment.
Conclusion
The majority of human cases of pulpal regeneration have thus
far had good clinical outcomes (absence of clinical signs and
symptoms, radiographic evidence of resolution of periapical
infections, continued root development and increased canal
wall thickness).
Most of the evidence thus far related to pulpal regeneration has
been based on case studies (low-level evidence) but the results
have been very promising. Current research is focused on ways
to be more selective in the type of tissue which develops in an
immature tooth by using various scaffolding, growth factors
and stem cells.
References
1) aae.org/colleagues (Regenerative Endodontics Spring 2013)
2) Banchs F, Trope M. Revascularization of immature perma-
nent teeth with apical periodontitis: new treatment protocol?
J Endod 2004;30:196-200.
3) Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative
endodontics: a review of current status and a call for action.
J Endod 2007;33:377-90.
4) Bohl KS, Shon J, Rutherford B, et al. Role of synthetic extra-
cellular matrix in development of engineered dental pulp. J
Biomater Sci Polym Ed 1998;9:749-64.
5) 25. Smith AJ, Scheven BA, Takahashi Y, et al. Dentine as a
bioactive extracellular matrix. Arch Oral Biol 2012;57:109-21.
6) 26. Sun HH, Jin T, Yu Q, et al. Biological approaches toward
dental pulp regeneration by tissue engineering. J Tissue Eng
Regen Med 2011;5:e1-16.
7) 1. Cvek M. Prognosis of luxated non-vital maxillary inci-
sors treated with calcium hydroxide and filled with gutta-
percha. A retrospective clinical study. Endod Dent Traumatol
1992;8:45-55.
Pulpal Regeneration,
continued
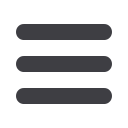
Post-op radiograph of
#9 pulpal regeneration.
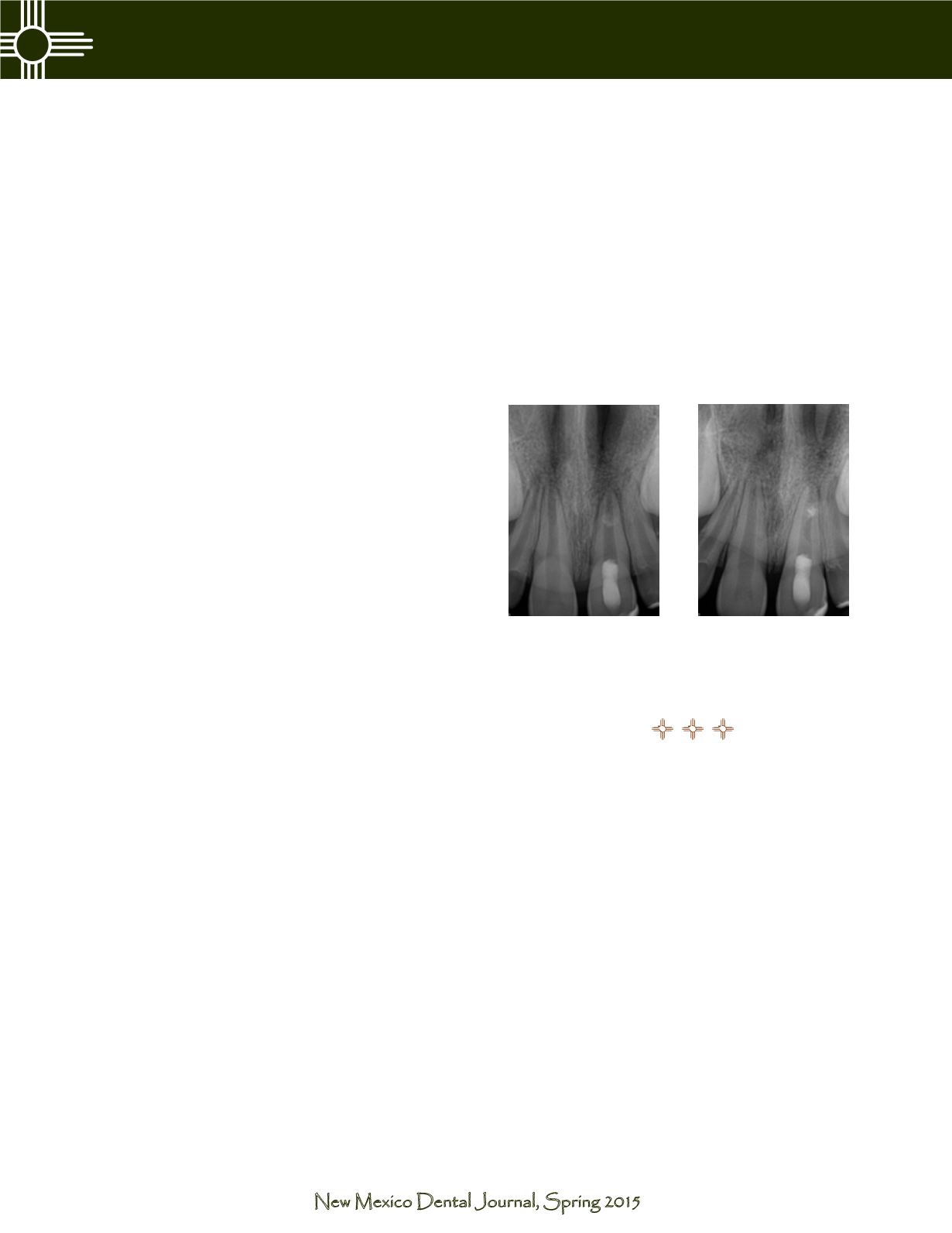
3-month recall of #9 pulpal
regeneration. Continued root
growth is expected at the 12
and 24-month recall exams.











