13
nmdental.org
for osteoporosis climbs to 0.21% after 4 years of therapy. The
osteoporotic patient is therefore at a 100 times lower risk than
those patients treated for cancer with bisphosphonate anti-
resorptive medication. In addition, the predominantly zole-
dronate cancer treated patient undergoing a tooth extraction
had a 33 fold increase for developing MRONJ according to
the position paper of 2014. Furthermore, the mandible has a
significantly higher incidence risk than the maxilla and females
are more predisposed than males although this last factor is
heavily influenced by a predominance of females receiving
these medications.
There is little data available
to support current recom-
mendations for a “drug holiday” prior to commencing dental
therapy according to the 2014 paper authored by Dr. Ruggerio
et al. A current American Dental Association Council on Scien-
tific Affairs recommendation suggested that patients receiving
lower cumulative doses of bisphosphonates (less than 2 years)
or denosumab could continue their antiresorptive medications
during invasive dental treatment. An international MRONJ
task force determined that bisphosphonate therapy greater than
4 years and comorbid risk factors to include smoking, rheu-
matoid arthritis, prior or current glucocorticoid therapy and/
or diabetes be evaluated for a drug holiday with consultation
with the prescriber of the bisphosphonate. Moreover, in 2011,
the FDA stated that there was “no substantial data to guide
decisions regarding the initiation or duration of a drug holiday.”
It may be best stated
that patients who are determined
in need of cancer related antiresorptive or antiangiogenic
drug treatment receive the same protocol as those in need of
head and neck radiation prior to the onset of such therapy. In
contrast, those receiving antiresorptive therapy for osteopo-
rosis/osteopenia be evaluated clinically and determined based
on individual clinical findings and documented comorbidities
whether they are at significant risk for developing MRONJ with
a specific dental procedure.
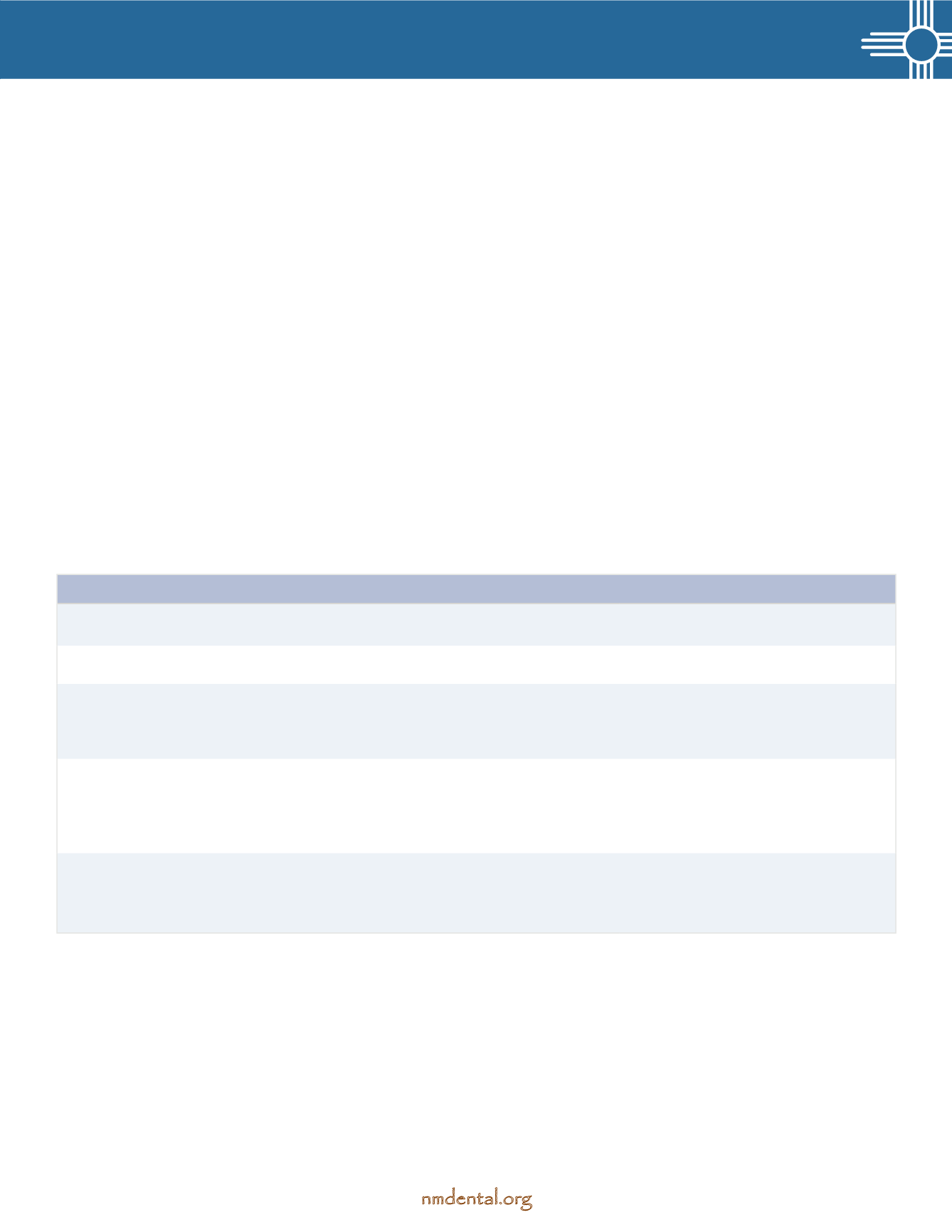
The following table
is copied here from Dr. Ruggerio et al
landmark article regarding Medication related osteonecrosis
of the jaw as presented in conjunction with the American
Association of Oral and Maxillofacial Surgeons. It is vital that
all dental practitioners are able to categorize and classify their
findings if faced with a possible diagnosis of MRONJ.
Staging of Medication-Related Osteonecrosis of the Jaw
*
Treatment Strategie
s †At risk
—no apparent necrotic bone in patients who have been
treated with oral or intravenous bisphosphonates
no treatment indicated
patient education
Stage 0
—no clinical evidence of necrotic bone but nonspecific
clinical findings, radiographic changes, and symptoms
systemic management, including use
of pain medication and antibiotics
Stage 1
—exposed and necrotic bone or fistulas that probes to bone in
patients who are asymptomatic and have no evidence of infection
antibacterial mouth rinse
clinical follow-up on a quarterly basis
patient education and review of indications
for continued bisphosphonate therapy
Stage 2
—exposed and necrotic bone or fistulas that probes to bone associated with infection as
evidenced by pain and erythema in the region of exposed bone with or without purulent drainage
symptomatic treatment with oral antibiotics
oral antibacterial mouth rinse
pain control
debridement to relieve soft tissue
irritation and infection control
Stage 3
—exposed and necrotic bone or a fistula that probes to bone in patients with
pain, infection, and ≥1 of the following: exposed and necrotic bone extending beyond the
region of alveolar bone (ie, inferior border and ramus in mandible, maxillary sinus, and
zygoma in maxilla) resulting in pathologic fracture, extraoral fistula, oral antral or oral nasal
communication, or osteolysis extending to inferior border of the mandible or sinus floor
antibacterial mouth rinse
antibiotic therapy and pain control
surgical debridement or resection for
longer-term palliation of infection and pain
*
Exposed or probeable bone in the maxillofacial region without resolution for longer than 8 weeks in patients treated with
an antiresorptive or an antiangiogenic agent who have not received radiation therapy to the jaws.
†
Regardless of disease stage, mobile segments of bony sequestrum should be removed without exposing uninvolved bone. Extraction of symptomatic
teeth within exposed necrotic bone should be considered because it is unlikely that extraction will exacerbate the established necrotic process.
Partial List of Antiresorptive Drugs:
Alendronate (Fosamax) oral
Denosumab (Prolia and Xgeva) SQ
Etidronate (Didronel) oral
Ibandronate (Boniva) oral/IV
Pamidronate (Aredia) IV
Risedronate (Actonel) oral
Zoledronic Acid
(Reclast Aclasta and Zometa) IV
References:
Ruggerio SL, Dodson, TB, Fontasia, J et al: American Association of Oral and Maxillofacial Surgeons Position Paper on Medication-Related Osteonecrosis of the Jaw—
2014 Update.
J Oral Maxillofacial surgery
72:1938. 2014
Ruggerio SL, Dodson, TB, Assael, LA et al: American Association of Oral and Maxillofacial Surgeons Position Paper on Medication-Related Osteonecrosis of the Jaw—
2009 Update.
J Oral Maxillofacial surgery
67:2. 2009