9
nmdental.org
S
ubcutaneous emphysema may occur during dental proce-
dures when using air water syringes or when using a high
speed, air driven drill. Subcutaneous emphysema has
been noted following common dental procedures including
endodontic treatment, restorative dentistry, periodontal
surgery and tooth extraction and is caused when compressed
air invades the soft tissues via a disrupted intraoral barrier such
as a laceration, incision, or a perforation through the dentoal-
veolar bone. The subcutaneous emphysema is usually restricted
to the tissue adjacent to the procedure site with an immediate
onset of swelling with crepitation. The area of emphysema is
usually non tender, without erythema and is treated conserva-
tively with observation and a short course of antibiotics. The
emphysema typically resolves over a period of seven to ten days
as the gas is resorbed into the blood stream.
The use of the high speed, air driven drill is especially
dangerous when surgically removing mandibular molars as
the roots are connected to the submandibular and sublingual
spaces which communicate with the parapharyngeal, deep
neck spaces, and ultimately to the mediastinum. Involvement
of the deep neck spaces may result in airway compromise and
may require intubation or a tracheotomy to secure the airway.
A 24 year old male with an unremarkable medical history
presented to the Emergency Department at the University of
Iowa Hospitals and Clinics with facial swelling. A high speed,
air driven drill was used to surgically remove the mandibular
left 2nd and third molars and mandibular right 2nd molar
three days prior to his presentation. He denied any facial
swelling prior to the procedure, but noticed significant swelling
immediately following. He returned to see his practitioner and
was promptly referred to the Emergency Department for an
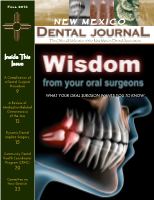
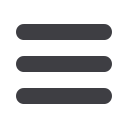
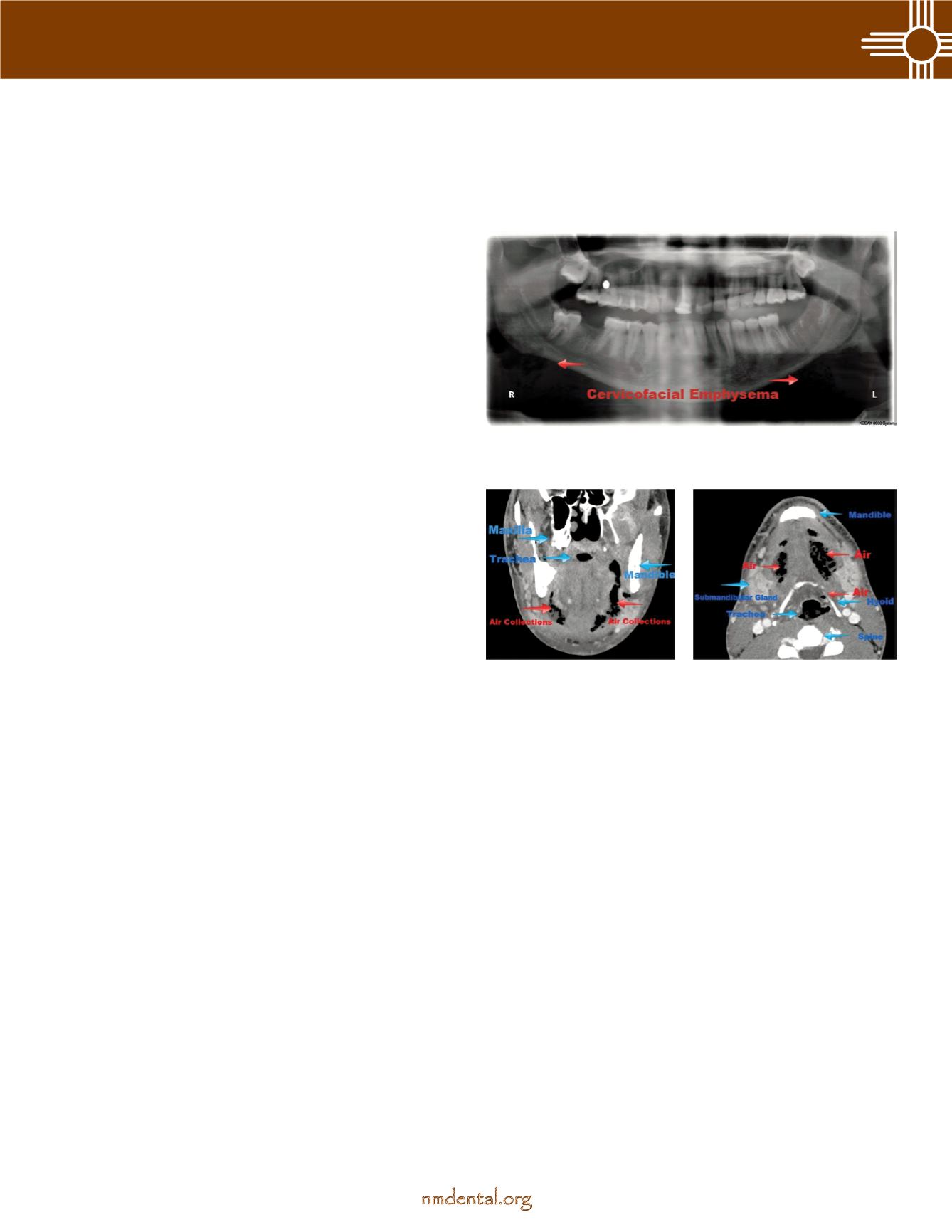
evaluation. Upon arrival a CT scan was obtained showing air
in the bilateral submandibular, submental, and lateral pharyn-
geal spaces. No airway obstruction was noted. A Panorex was
also obtained showing the extraction sites of the mandibular
left 2nd and third molars and mandibular right 2nd molar
showing no tooth fragments to be present. Emphysema was
appreciated on the Panorex. He denied any dysphagia, dyspnea,
fever, or chills. He did not have any difficulties opening and
reported moderate mandibular pain. He was tolerating his oral
secretions and was not in any distress. Bilateral submandibular
and submental firmness without fluctuance was noted. His
uvula was midline and minimal lateral pharyngeal swelling was
present. The floor of his mouth was soft without sublingual
edema. No crepitus was appreciated in the face or neck. He was
afebrile and his WBC count was normal. He was admitted for
observation, IV antibiotics, steroids, pain control, and fluids.
His clinical picture improved significantly during his hospital
stay and he was discharged on hospital day four.
He returned to Emergency Department three days later with
increased facial swelling, dyspnea, difficulties tolerated his
oral secretions, dysphonia, and trismus. He reported that he
was not able to fill his antibiotic prescription and that his
swelling had increased significantly over the past 24 hours.
A new CT was obtained showing large fluid collections in
the bilateral masticator, pterygomandibular, submandibular,
submental, sublingual, lateral pharyngeal, and pretracheal
spaces extending to the mediastinum. He was taken imme-
diately to the operating room where his airway was secured
with an orotracheal tube. A surgical team consisting of Oral
and Maxillofacial Surgery, Otolaryngology and Thoracic and
Cardiovascular Surgery explored the involved facial spaces and
mediastinum. Drains were placed appropriately. The patient
was admitted to the Surgical and Neuroscience Intensive Care
Unit where he remained intubated for approximately five days.
His hospital admission continued for another two weeks for
continued observation, sepsis management, IV antibiotics, and
pain control prior to his discharge.
By Brett Schow, DDS—Bear Canyon Oral and Facial Surgery
AComplication of a Dental Surgical Procedure
Figure 1. Post extraction Panorex showing cervicofacial
emphysema as indicated by the red arrows.
Figure 2. Initial coronal
computed tomography
scan showing anatomy
and air collections.
Figure 3. Initial axial
computed tomography
scan showing anatomy
and air collections.
continues