10
New Mexico Dental Journal, Fall 2016
Cervicofacial emphysema, as demonstrated with this case, is
rare, but can occur when using a high speed, air driven drill
to surgically removal teeth, especially mandibular molars. The
high speed, air driven drill introduces pressured air, non-sterile
water and contaminated debris from the surgical wound into
the subcutaneous and soft tissues. This is especially dangerous
when surgically removing mandibular molars as the roots are
connected to the submandibular and sublingual spaces which
communicates with the parapharyngeal, deep neck spaces,
and ultimately to the mediastinum. Once air enters the medi-
astinum it may involve the pleural cavity, pericardium, and
retroperitoneum. Involvement of the deep neck spaces may
compromise the airway and patients who demonstrate difficul-
ties breathing should be referred immediately to the Emergency
Department for evaluation. Most incidences of subcutaneous
emphysema will resolve after seven to ten days of conservative
treatment that may include antibiotics, corticosteroids, and
pain management. These patient should be followed closely
and referred appropriately with any increases in swelling or
breathing difficulties.
This case demonstrating the development and spread of the
infection from the oral cavity, through the fascial and deep
neck spaces to the mediastinum is called descending necro-
tizing mediastinitis. Descending necrotizing mediastinitis is
usually associated with those who are immunosuppressed and
is known to have a mortality rate of 20–40%. Descending
necrotizing mediastinitis requires aggressive surgical treatment.
In this case, a multi-specialty team of surgeons accessed the
deep neck spaces and the mediastinum via intraoral and tran-
scervical approaches to allow for appropriate drainage of the
collections. The bacteria involved in descending necrotizing
mediastinitis typically consist of the aerobic and anaerobic
bacteria commonly found in the oral cavity. This was in accor-
dance with the cultures from this case and a broad spectrum
antibiotic regimen, consisting of IV Vancomycin and Unasyn,
was given per Infectious Disease recommendations.
Cervicofacial emphysema can rapidly progress to infection
involving the deep spaces of the neck and requires close
observation and aggressive surgical intervention as necessary.
The careful use of the air water syringe and the high speed,
air-driven drill while performing routine dental procedures is
necessary to avoid or minimize any complications that may be
potentially life threatening. Referral for appropriate care and
management of subcutaneous emphysema may be necessary
particularly with any involvement of the deep neck spaces that
can potentially result in airway compromise.
References
1. SC Chen, FY Lin, KJ Chang: Subcutaneous emphysema and pneumomedi-
astinum after dental extraction.
Am J Emerg Med
, 17 (1999), pp. 678–680.
2. S. Kinzer, J. Pfeiffer, S. Becker, G.J. Ridder. Severe deep neck space infections
and mediastinitis of odontogenic origin: clinical relevance and implications
for diagnosis and treatment.
Acta Otolaryngol
, 129 (2009), pp. 62–70.
3. JO Capes, JM Salon, DL Wells. Bilateral cervicofacial, axillary, and anterior
mediastinal emphysema: a rare complication of third molar extraction.
J Oral
Maxillofac Surg
, 57 (1999), pp. 996–999.
4. P. Mihos, K. Potaris, I. Gakidis, D. Papadakis, G. Rallis. Management
of descending necrotizing mediastinitis.
J Oral Maxillofac Surg
, 62 (2004),
pp. 966–972.
5. Abdelkarim Shimi, Said Benlamkaddem, Driss Tahse, Ali Derkaoui,
Mohammed Khatouf. Cervicofacial Emphysema and Pneumomedias-
tinum Complicating a Dental Extraction. DOI: 10.4236/crcm.2015.47051,
pp. 257-260.
AComplication of a Dental Surgical Procedure,
continued
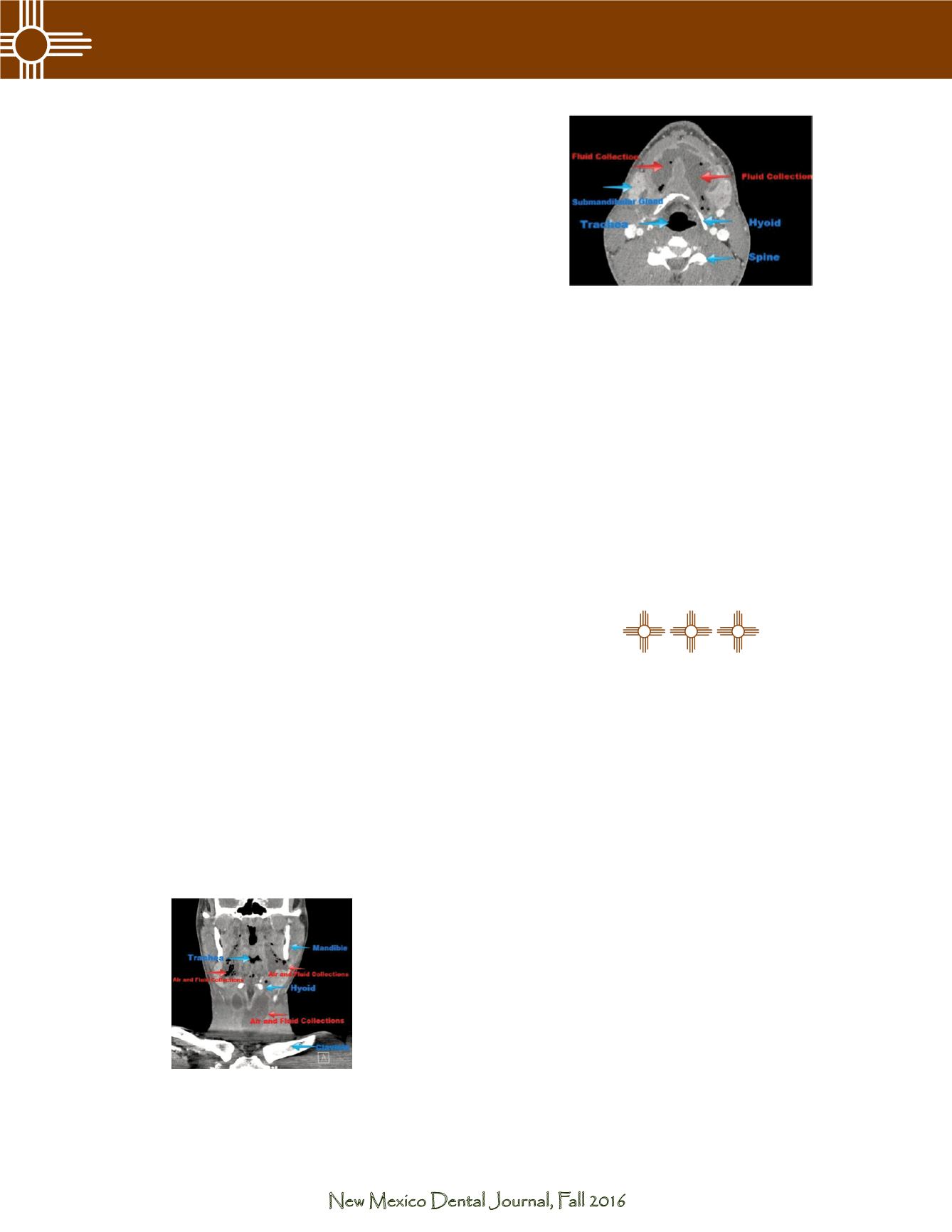
Figure 4. Subsequent coronal computed tomography
scan showing anatomy and fluid collections.
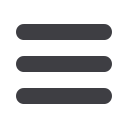
Figure 5. Subsequent axial computed tomography
scan showing anatomy and fluid collections.