Why do patients need navigation
and case management?
Case management has been defined as
the coordination of care that a patient
may need to maximize access to care and
their overall health outcomes. This in-
cludes explaining the procedure in plain
language, ensuring transportation to the
appointment, arranging translation ser-
vices as needed, and following up with
support services. As much as most den-
tists like to think that patients under-
stand what treatment they need, studies
prove that not to be true in many cases!
In some circumstances, patients with
commercial insurance may not know
how to access a dental office. Just pick-
ing up the phone and making an ap-
pointment can be confusing and over-
whelming for many people. They may
be unsure of which dental office accepts
their insurance and how to begin a treat-
ment series.
The existing CDHCs help patients find
dental offices that accept their insur-
ance, have office hours that fit their
work or school schedules, and answer
questions regarding how long the treat-
ment may be take. With community
mapping, oral health promotion and
program eligibility being integral ele-
ments within the CDHC courses, pa-
tients can be navigated not only into
public health clinics, but into private
practices as well.
These personalized navigational skills
have been shown to greatly reduce pa-
tient no show rates. As community
health centers and public health clinics
well know, patients expressed many bar-
riers to keeping appointments. CDHCs
are trained to effectively reduce those
rates and track patients to completion.
Medical-Dental Collaboration is a
prime area where a CDHC can assist
patients. As the ADA and the American
Academy of Pediatric Dentistry have
stated, the first dental visit should hap-
pen by 12 months of age. Many pediatri-
cians appreciate this policy, but guiding
parents and young patients to dental
homes typically involves only the pedia-
trician making the suggestion. With a
CDHC visiting the office of a pediatri-
cian in person, families may be directly
appointed into the dental schedule of
an office.
CDHCs often spend time in nursing
homes or assisted living facilities per-
forming oral health screening services
and making referrals to a dental office.
Of added value is the CDHCs ability to
provide in-service training to nursing
home personnel on oral health care and
denture maintenance.
The ADA and the American College of
Obstetrics and Gynecology collaborated
on a Joint Consensus Statement several
years ago that reinforced the safety fac-
tors in having pregnant women receive
dental care throughout their pregnancy.
This largely unknown information,
coupled with the uncertainty of locat-
ing dental services, can be enhanced by
a CDHC who could provide oral health
education and navigation to these preg-
nant women.
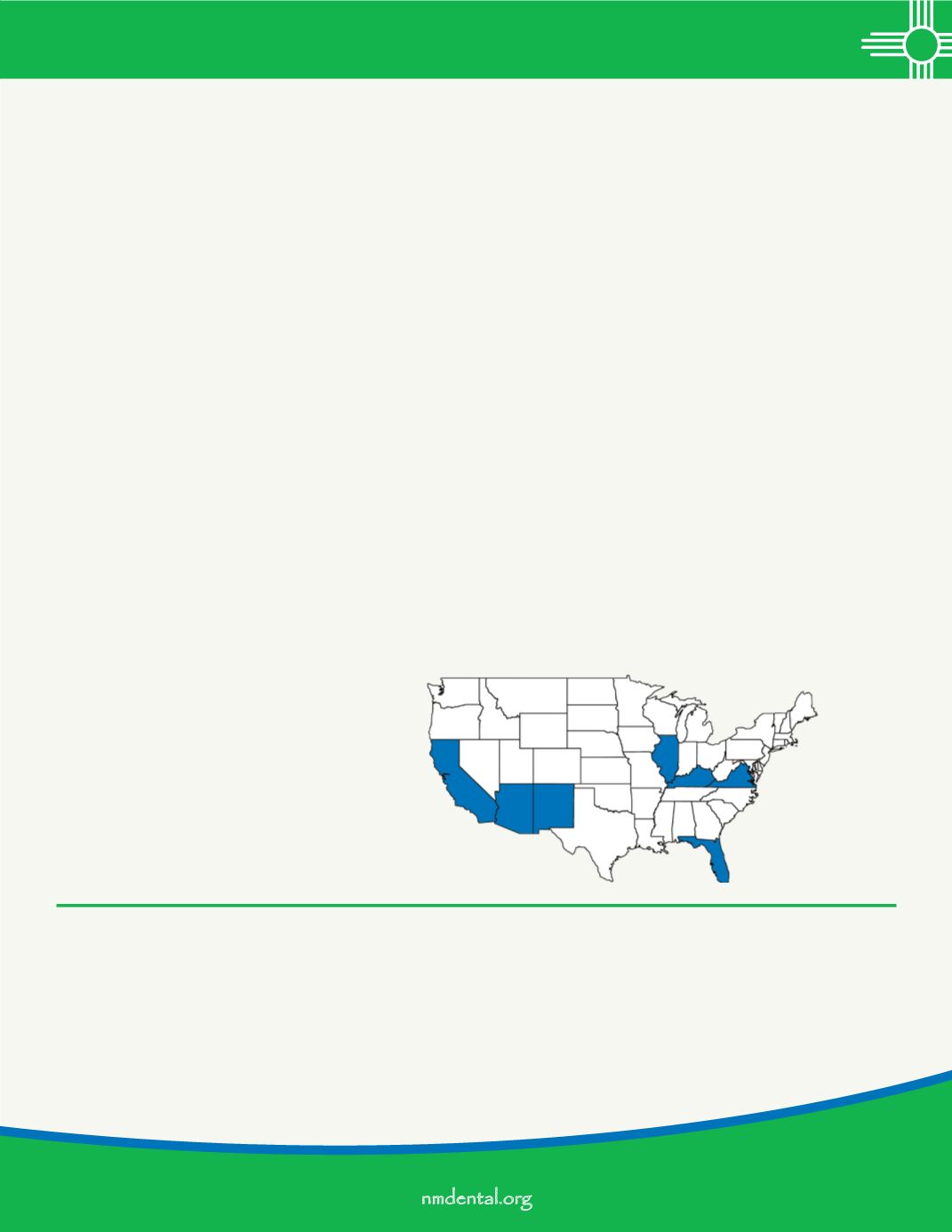
There are now seven states that are of-
fering or will soon offer the CDHC pro-
gram: California, Arizona, New Mexico,
Illinois, Virginia, Florida, and Kentucky.
The Central New Mexico Community
College will begin their second class in
early 2017.
N
ew Mexico has been at the forefront nationally in the development and implementation of the Community Dental
Health Coordinator (CDHC). In 2011, the New Mexico legislature approved certifying CDHC’s as part of the Dental
Health Care Act. In 2013, the NMDA/ADA undertook a demonstration project at Hidalgo Medical Services, Silver
City, with Lori Wood from Pennsylvania providing CDHC services. Subsequently, Wood becomes the first person in the na-
tion to receive CDHC certification from a state dental board, issued from the New Mexico Board of Dental Health. Central
New Mexico Community College (CNM) became the first “bricks & mortar” CDHC training program in the nation outside
of the ADA’s pilot project, launching their program in August 2014. CNM graduated their first students in 2015.
The next class will begin in January 2017 and is seeking more applicants.
21
nmdental.org