 www.ohca.com
www.ohca.com
Spring/Summer 2017
The Oregon Caregiver
13
QUALITY
anecdotal information from what
is really happening using objective
information. For example, a leader may
perceive that staff satisfaction is high in
an organization. Measuring it routinely
with a consistent, objective tool will
provide valuable information
and insights that would not
necessarily be revealed
through remarks from some
staff or general perception.
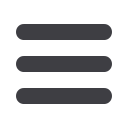
It follows that quality in
a long term care setting
should not be solely based
on one licensing survey, a
single complaint investigation,
or other regulatory factors. A
holistic review of quality long term care
is rooted in these foundational metrics:
resident and family satisfaction, staff
satisfaction, compliance with applicable
rules and standards, clinical data, and
profession-standard quality indicators.
Currently, this holistic measurement
model only partially exists in
Oregon’s long term care system.
Federal regulations for nursing
facilities and assisted living do require
quality assurance and performance
improvement programs (referred to
as QAPI), and, in the past decade, the
Centers for Medicare and Medicaid
Services (CMS) has routinely enhanced
guidelines for nursing facilities quality
measurement. These QAPI programs
take a systematic, comprehensive, and
data-driven approach to maintaining and
improving safety and quality in nursing
homes while involving all nursing home
caregivers in practical and creative
problem solving.
In these regulations, quality assurance
(QA) includes the specification of
standards for quality of service and
outcomes as well as a process throughout
the organization for assuring that
care is maintained at acceptable levels
in relation to those standards. QA is
on-going and both anticipatory and
retrospective in its efforts to identify how
the organization is performing, including
where and why facility performance is at
risk or has failed to meet standards.
Performance improvement (PI) refers to
the continuous study and improvement
of processes. Additionally, it considers
the intent to better services or outcomes
and prevents or decreases the likelihood
of problems by identifying areas of
opportunity and testing new approaches
to fix underlying causes of persistent/
systemic problems or barriers to
improvement. PI can and should make
good quality care even better.
As a result, QAPI amounts to much
more than a provision in federal statute
or regulation; it represents an ongoing,
organized method of doing business to
achieve optimum results for those served
and the organization.
The QAPI model has been
adapted for community based
care and is currently being
piloted in Oregon assisted
living and residential care
communities through
CareOregon’s LiveWell
method initiative. LiveWell
is a quality assurance and
performance improvement
methodology focused on
empowerment of staff. The preliminary
results are starting to emerge, and
participants have already begun using
and analyzing their data to improve
quality care, reduce costs, improve staff
retention and regulatory compliance, and
enhance resident well-being.
As this program and other data
gathering, or QAPI, initiatives
throughout Oregon’s long term care
sector show, using thoughtful and
holistic data can do so much good
for communities, most of all by
improving the quality provision of care
and enhancing resident and family
satisfaction.
Linda Kirschbaum is the Senior VP of Quality Services at OHCA.