» A magazine for and about Oregon Community Hospitals.
24
Working Together
BAY AREA HOSPITAL’S SHARED GOVERNANCE MODEL INCREASES PATIENT SAFETY
HOSPITAL SPOTLIGHTS, CONT.
It sounds more confusing than it really is: shared
governance is just another way to think about patient safety.
For the nurses at
Bay Area Hospital
in Coos Bay, it is an
organizational model that goes much deeper. But what it
boils down to is a process that allows patients to have a say
in how their care is administered.
Amanda Bernetz, RN, who works on the medical care unit,
explained it as a way frontline workers and executives go
about “working together on how we work here—on how the
nurses function here in our jobs.”
The organizational model works through a number of
different subgroups in each unit in the hospital. For
instance, the nurses gather regularly in their unit to look for
ways to improve workflow. There are also teams that focus
primarily on improving patient safety within those units.
Jennifer Green, RN, the clinical nurse manager of the
hospital’s post-surgical unit, doesn’t want the community
to get lost in the process, however; she wants them to
remember that when they come to the hospital, they are
getting the safest care.
The safety program allows for defects to be caught before a
problem actually occurs. These days, a near-miss is enough
to elicit change.
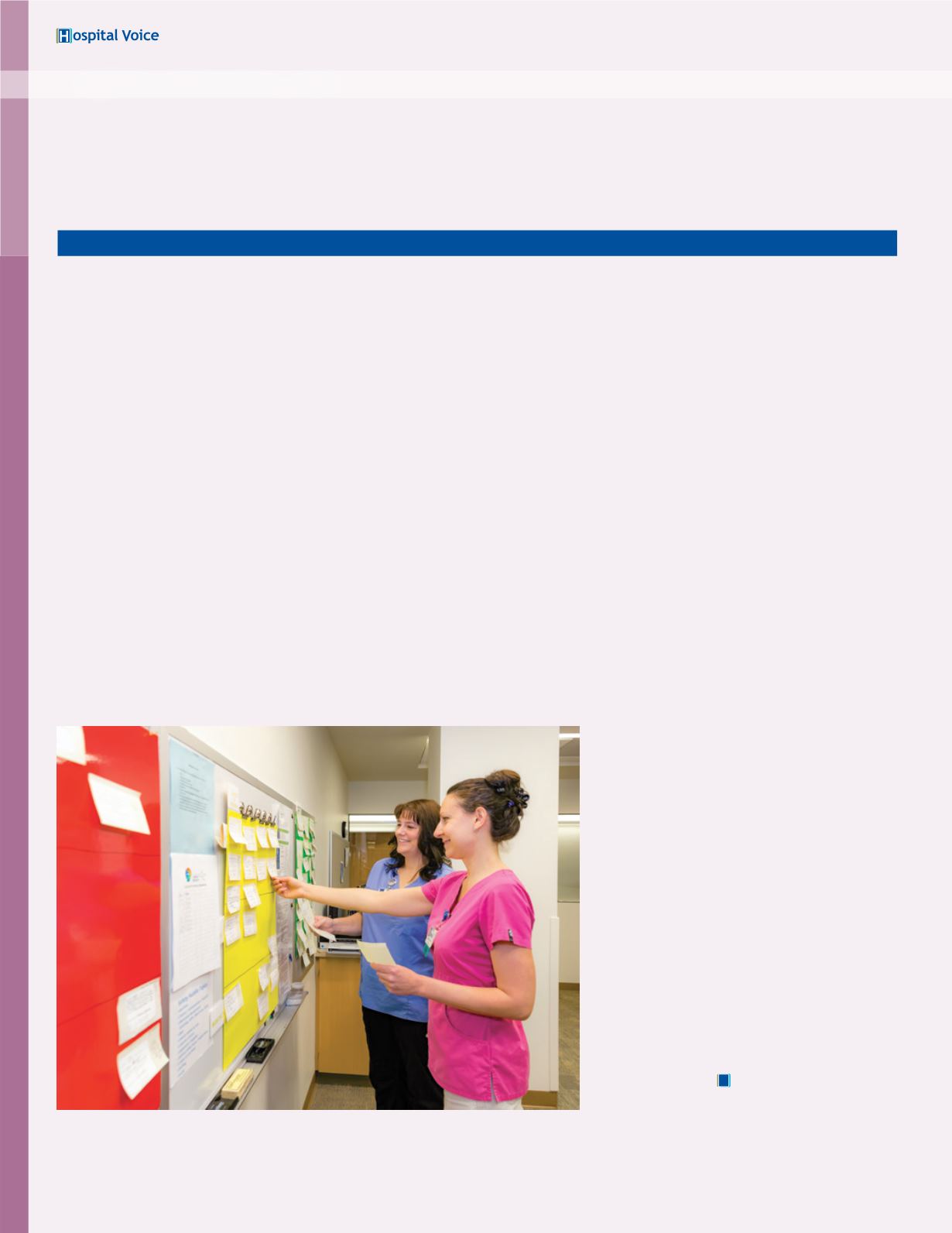
Daily “safety huddles” help identify issues that need to be
addressed before they become major problems. A color-
coded board helps keep the units on task. New defects are
designated in red. The yellow board is work in progress.
Green signifies completed projects. The many success stories,
which show up in blue, indicate that the effort is effective.
“Without shared governance the nurses wouldn’t feel
empowered to speak up and advocate for our patients,” said
Kristen Hyatt, RN, a nurse on the intensive care unit. “Now
when we see something our patients need or something that
isn’t working for them, nurses have that frontline power—
we can say what we need for patients and it gets done. These
programs help facilitate that.”
Some changes that have benefited patients may go largely
unnoticed by them, such as “Quiet Zone” mats that allow
for nurses to have uninterrupted time when they access
patient medications from the pharmacy cart, or moving
refrigerators to keep cold water closer to
patients who request it.
One change that has come about through
this new empowerment allows patients and
their families to have a greater say in their
care. Deanna Prater, RN, the hospital’s
nursing excellence coordinator, said it
was thanks to this emphasis on shared
governance that bedside reports became a
reality.
“Doing a report at the bedside, rather than
in a room without the patient or family
there, makes so much sense,” she said.
“Bedside reports are an opportunity to
involve the patient and family when nurses
are giving the change-of-shift report, so
patients and families can be involved to say
‘This is a concern of ours.’ It’s just better
communication.”
H
During a safety huddle, Tabitha Myers, RN, and Angela Haines, RN,
update a work in progress on the yellow board.


















